The GI Map, a sensitive at home stool test, has helped me find infections that are otherwise hard to test for, such as parasites, candida and h. Pylori.
The GI Map is extremely useful because it analyzes the biome of the large intestine and the biome of the stomach, while also measuring immunity, inflammation, digestion, liver function, leaky gut and gluten sensitivity.
In the h. Pylori rescue guide, I talk about how to use the GI Map to spot a hidden h. pylori infection. In this blog post, I show how to use the GI Map to determine if a low level h. pylori infection, that is in the normal range, should be addressed.
The GI Map’s efficacy is based on locating DNA traces of pathogens. But sometimes, h. Pylori can also hide on the GI Map test or show up as low when the actual levels are much higher.
But the benefit of the GI Map is that is offers a big picture view of what effect h. pylori could be having on the biome.
Even what shows up as a mild h. pylori infection on the test could still be causing problems in the biome and gut symptoms.
H. pylori is hard to test for because it sheds unevenly in the stool and is protected by biofilm. A low or normal amount of h. pylori could just be a reading on what is living outside of the biofilm. Most of the infection is hiding behind biofilm.
Biofilm is made from proteins and biological material by bacteria and yeast in the gut, both good and bad guys, to protect from eradication by the immune system.
Some practitioners are not aware that the biofilm could be hiding the bulk of the infection and ignore low positive h. pylori results. And this could be a huge mistake.
Let’s look at a current case study where I break down how I know whether or not to address h. pylori naturally.
I also take symptoms into account, but below we look at how to use the GI Map to get more useful information.
Client case study
Lorena came to me complaining of stomach pains after eating. This is a common h. pylori symptom. While it had only been going on for 3 months, she also had a past history of an ulcers. This is also often caused by h. pylori.
Unfortunately, all of the multiple tests she did at her doctor’s office showed she was negative for h. Pylori. So she was thrown off track for years of the root cause for her current pain and past ulcer.
She was confused, in pain and losing weight because she was afraid to eat anything.
We ran a GI Map stool test.
Her GI Map revealed a low positive for h. Pylori with no virulent strains. Virulent strains (also called virulence factors) are nastier and more aggressive strains of h. pylori that can cause ulcers or more rarely cancer of the stomach. If there’s a virulent strain, I always recommend addressing h. pylori to matter what level is shows up.
There are markers on the GI Map that tell me if h. pylori is compromising digestion, lowering pathogen protection and stressing the biome. I go over some of them below, but there are more in the h. pylori guide.
Three clues h. pylori is a problem
Three things tipped me off that h. Pylori was causing problems for my client.
- Certain bacteria that flagged high.
- A parasite that is associated with h. pylori.
- Low pancreatic enzymes.
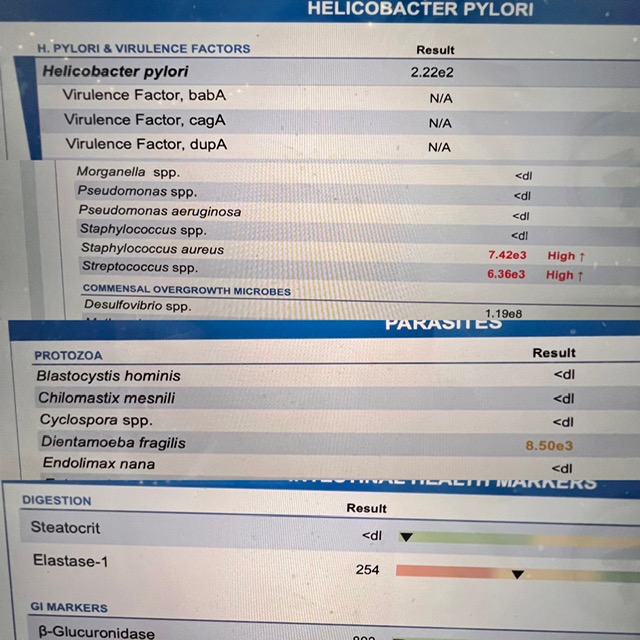
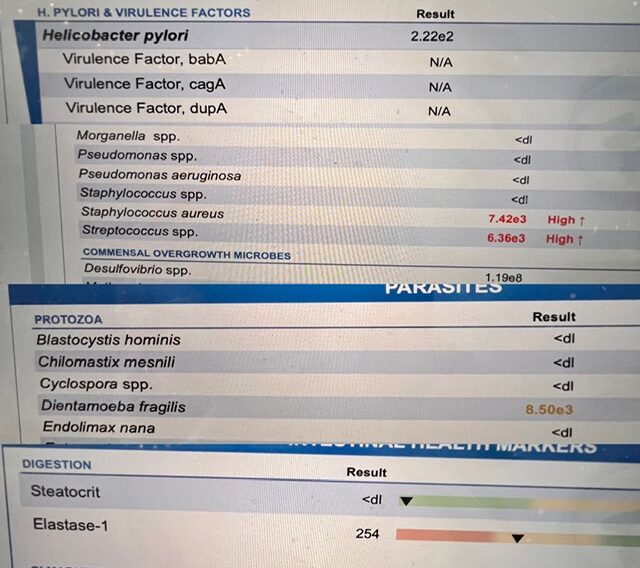
The first of the 4 images above show Lorena’s h. pylori level, which looks like it is in range.
The second image show staph and strep overgrowth.
Staph and strep are typically elevated when h. pylori lowers stomach acid. This is because they both live in the mouth and when they are swallowed they should be destroyed by stomach acid. When stomach acid is low, they end of in the large intestine, where they overgrow.
The third image shows that she was positive for a parasite.
There are two parasites I commonly see with h. Pylori, blastocystis hominis and/or dientamoeba fragilis. She has dientamoeba.
The last image showed low enzymes.
Elastase is the marker for digestive enzymes. When it is low it means stomach acid is low. Stomach acid signals the pancreas to produce enzymes for digestion. When stomach acid is low it does not signal the pancreas to produce enough enzymes for healthy digestion.
With low stomach acid and low enzymes you can’t digest your food properly, which can result in bloating, lack of appetite, reflux, gas, feeling full after eating a little, the sensation of food sitting in your stomach, food sensitivities or constipation.
H. Pylori is the most common cause of low stomach acid, but high chronic stress and advanced age can also lower stomach acid.
Lorena was in her 40s and not particularly stressed, so the cause of her low stomach acid was h. Pylori.
To address her symptoms we started with a month of matula tea and followed up with a month of mastic gum with biofilm buster. You can find the full mastic gum protocol in Fullscript (just search for my h. pylori protocol) or in my guide.
Note: While mastic gum is safe for most people, always work with a practitioner when beginning any new supplement protocol for your safety.
Our plan is to tackle h. Pylori first for two month.
Then we address Lorena’s parasite.
The last step is healing and sealing her gut lining with probiotics and a glutamine-based repair powder.
This is a sneak peek at how I work, and use tests like the GI Map to guide my protocols. Also it is important to address pathogens in the right order.
H. Pylori is always addressed first.
And you can’t address everything at once because the immune system will be stretched too thin and protocol efficacy will suffer.
Testing may be expensive but it saves guess work, time, energy and money in the end.
I posted this reel on Instagram summing up what I wrote here.
Follow me on Instagram for more tips and digestive health advice, if you found this post useful.